Onychomycosis
Abstract
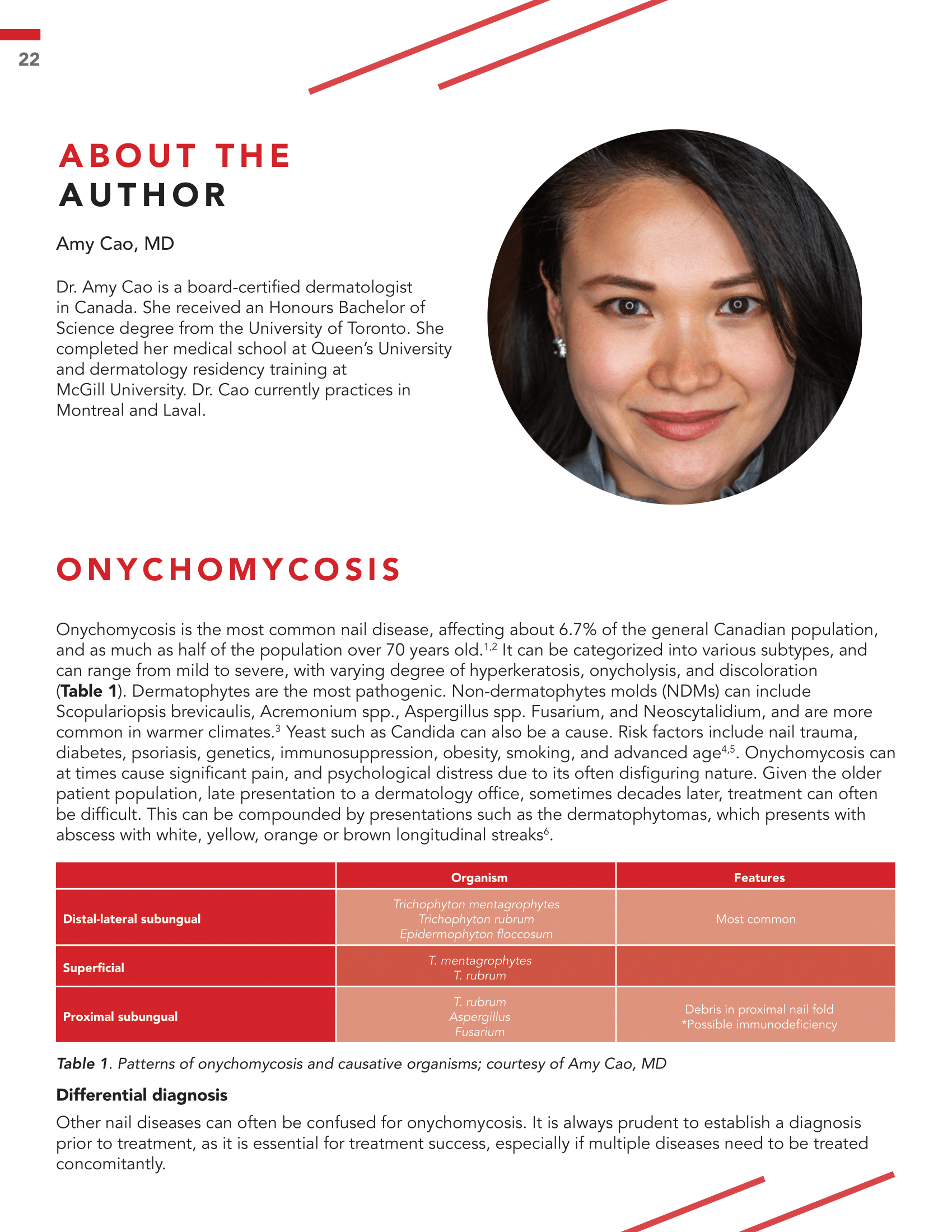
Onychomycosis is the most common nail disease, affecting about 6.7% of the general Canadian population, and as much as half of the population over 70 years old. It can be categorized into various subtypes, and can range from mild to severe, with varying degree of hyperkeratosis, onycholysis, and discoloration. Dermatophytes are the most pathogenic. Non-dermatophytes molds (NDMs) can include Scopulariopsis brevicaulis, Acremonium spp., Aspergillus spp. Fusarium, and Neoscytalidium, and are more common in warmer climates. Yeast such as Candida can also be a cause. Risk factors include nail trauma, diabetes, psoriasis, genetics, immunosuppression, obesity, smoking, and advanced age. Onychomycosis can at times cause significant pain, and psychological distress due to its often disfiguring nature. Given the older patient population, late presentation to a dermatology office, sometimes decades later, treatment can often be difficult. This can be compounded by presentations such as the dermatophytomas, which presents with abscess with white, yellow, orange or brown longitudinal streaks.
References
Gupta AK, Gupta G, Jain HC, et al. The prevalence of unsuspected onychomycosis and its causative organisms in a multicentre Canadian sample of 30,000 patients visiting physicians offices. J Eur Acad Dermatol Venereol. 2016;30(9):1567-1572.
Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther. 2010;35(5):497–519.
Svejgaard EL, Nilsson J. Onychomycosis in Denmark: prevalence of fungal nail infection in general practice. Mycoses. 2004;47:131-135.
Elewski BE. Onychomycosis: pathogenesis, diagnosis, and management. Clin Microbiol Rev. 1998;11:415–429.
Gupta A, Lynde CW, Jain HC et al. A higher prevalence of onychomyco- sis in psoriatics compared with non-psoriatics: a multicentre study. Br J Dermatol. 1997;136:786–789.
Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol. 2010;24:679–684.
Klaassen KMG, Dulak MG, Van De Kerkhof PCM, Pasch MC. The prevalence of onychomycosis in psoriatic patients: a systematic review. J Eur Acad Dermatol Venereol. 2014;28(5):533-541.
Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2013;27:509-513.
Koshnick RL, Lilly KK, St Clair K, Finnegan MT, Warshaw EM. Use of diagnostic tests by dermatologists, podiatrists and family practitioners in the United States: pilot data from a cross-sectional survey. Mycoses. 2007;50(6):463-469.
Gupta AK, Elewski BE, Rosen T, et al. Onychomycosis: strategies to minimize recurrence. J Drugs Dermatol. 2016;15(3):279-282.
Sakamoto M, Sugimoto N, Kawabata H, et al. Transungual delivery of efinaconazole: its deposition in the nail of ony- chomycosis patients and in vitro fungicidal activity in human nails. J Drugs Dermatol. 2014;13(11):1388-1392.
Wilsmann-Theis D, Sareika F, Bieber T, Schmid-Wendtner MH, Wenzel J. New reasons for histopathological nail-clipping examination in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2011;25(2):235-237.
Arrese JE, Pierard-Franchimont C, Greimers R, Pierard GE. Fungi in onychomycosis. A study by immunohistochemistry and dual flow cytometry. J Eur Acad Dermatol Venereol. 1995;4:123–130.
Lipner SR, Scher RK. Prognostic factors in onychomycosis treatment. J Infect Dis Ther. 2015;3:202.
US Food and Drug Administration. Medical devices and clinical trial design for the treatment or improvement in the appearance of fungally-infected nails—draft guidance for industry and FDA staff. 2015. http://www.fda.gov/downloads/ MedicalDevices/DeviceRegulationandGuidance/ GuidanceDocuments/UCM431312.pdf. Accessed 2021 Sep 1.
Kreijkamp-Kaspers S, Hawke K, Guo L, Kerin G, Bell-Syer SEM, Magin P, Bell-Syer SV, van Driel ML. Oral antifungal medication for toenail onychomycosis. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.:CD010031.
Korting HC, Schollmann C. The significance of itraconazole for treatment of fungal infections of skin, nails and mucous membranes. J Dtsch Dermatol Ges. 2009;7(11-19):11-20.
Gupta AK, Ryder JE, Johnson AM. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol. 2004;150(3):537-544.
https://www.ask.novartispharma. ca/download.htm?res=lamisil_scrip_e. pdf&resTitleId=728Accessed; Sept 14, 2021.
Sigurgeirsson B, Olafsson JH, Steinsson JB, Paul C, Billstein S, Evans EGV. Long-term effectiveness of treatment with terbinafine vs itraconazole in onychomycosis: a 5-year blinded prospective follow-up study. Arch Dermatol. 2002;138(3):353-357.
Gupta AK, Konnikov N, Lynde CW. Single-blind, randomized, prospective study on terbinafine and itraconazole for treatment of dermatophyte toenail onychomycosis in the elderly. J Am Acad Dermatol. 2001;44:479-484.
Gupta AK, Baran R, Summerbell R. Onychomycosis: strategies to improve efficacy and reduce recurrence. J Eur Acad Dermatol Venereol. 2002;16:579-586.
Sigurgeirsson B, Paul C, Curran D, Evans EG. Prognostic factors of mycological cure following treatment of onycho- mycosis with oral antifungal agents. Br J Dermatol. 2002;147:1241-1243.
Foley K, Gupta AK, Versteeg S, Mays R, Villanueva E, John D. Topical and device-based treatments for fungal infections of the toenails. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No.:CD012093.
Lecha M, Effendy I, Feuilhade de Chauvin M, Di Chiacchio N, Baran N. Treatment options-development of consensus guidelines. J Europ Acad Dermatol Venereol. 2005;19 Suppl 1:25–33.
Jubilia (efinaconazole) topical solution, 10% [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals. Available at: http://www.valeant.com/Portals/25/Pdf/PI/Jublia-PI.pdf. Accessed Sept 14, 2021.
Kerydin (tavaborole) topical solution, 5% [package insert]. Melville, NY: Fougera Pharmaceuticals. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/ label/2014/204427s000lbl.pdf. Accessed Sept 14, 2021.
Penlac nail lacquer (ciclopirox) topical solution, 8% [package insert]. Bridgewater, NJ: Dermik Laboratories. Available at: http://products.sanofi.us/penlac/penlac.html. Accessed Sept 14, 2021.
Eichenfield LF, Elewski B, Sugarman JL, Rosen T, Vlahovic TC, Gupta AK, Gold LS, Pillai R, Guenin E. Safety, pharmacokinetics, and efficacy of efinaconazole 10% topical solution for onychomycosis treatment in pediatric patients. J Drugs Dermatol. 2020;19(9):867-872.
Shemer A, Gupta AK, Kamshov A, et al. Topical antifungal treatment prevents recurrence of toenail onychomycosis following cure. Dermatol Ther. 2017;30.
Watanabe D, Kawamura C, Masuda Y, Akita Y, Tamada Y, Matsumoto Y. Successful treatment of toenail onychomycosis with photodynamic therapy. Arch Dermatol 2008;144:19–21.
Jennings MB, Pollak R, Harkless LB, Kianifard F, Tavakkol A. Treatment of toenail onychomycosis with oral terbinafine plus aggressive debridement: IRON-CLAD, a large, randomized, open-label, multicenter trial. J Am Podiatr Med Assoc. 2006;96(6):465-473.