An Update on Pediatric Alopecia Areata
Abstract
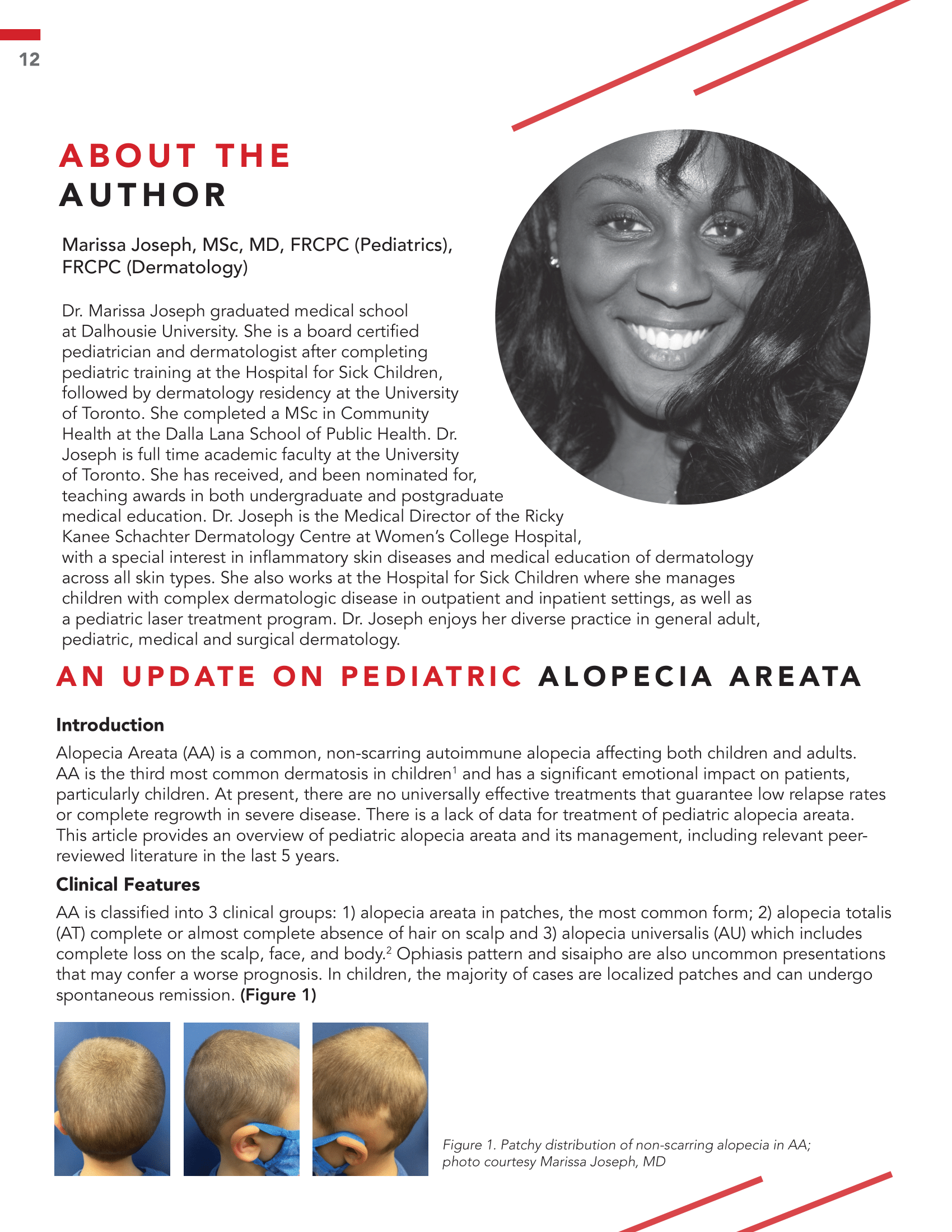
Alopecia Areata (AA) is a common, non-scarring autoimmune alopecia affecting both children and adults. AA is the third most common dermatosis in children and has a significant emotional impact on patients, particularly children. At present, there are no universally effective treatments that guarantee low relapse rates or complete regrowth in severe disease. There is a lack of data for treatment of pediatric alopecia areata. This article provides an overview of pediatric alopecia areata and its management, including relevant peer-reviewed literature in the last 5 years.
References
Wohlmuth-Wieser, Iris, et al. “Childhood alopecia areata—data from the National Alopecia Areata Registry.” Pediatric Dermatology. 2018 Mar;35(2):164-169. doi: 10.1111/pde.13387. Epub 2018 Jan 15.
Juárez-Rendón, Karina J., et al. “Alopecia areata: Actualidad y perspectivas.” Archivos argentinos de pediatria. 2017;115(6):e404-e411.
Patel D, Li P, Bauer AJ, Castelo-Soccio L. Screening guidelines for thyroid function in children with alopecia areata. JAMA Dermatol. 2017;153(12):1307-1310.
Mahmoudi H, Salehi M, Moghadas S, Ghandi N, Teimourpour A, Daneshpazhooh M. Dermoscopic findings in 126 patients with alopecia areata: A cross-sectional study. Int J Trichology. 2018;10(3):118-123.
Donovan J. Donovan medical trichoscopy. https://donovanmedical.com/trichoscopy.
Burnat AW, et al. “Trichoscopy of alopecia areata in children. A retrospective comparative analysis of 50 children and 50 adults.” Pediatric Dermatology. 2019;36(5):640-645.
Liu, Lucy Y, et al. “Tofacitinib for the treatment of severe alopecia areata and variants: a study of 90 patients.” Journal of the American Academy of Dermatology. 2017;76(1):22-28.
Nawaf A, Nour TM, Hussain NH. “Janus kinase inhibitors for the treatment of severe alopecia areata: an open-label comparative study.” Dermatology. 235(2):130-136.
Phan K, Sebaratnam DF. “JAK inhibitors for alopecia areata: a systematic review and meta-analysis.” Journal of the European Academy of Dermatology and Venereology. 2019 May;33(5):850-856.
Liu LY, King BA, Craiglow BG. “Alopecia areata is associated with impaired health-related quality of life: a survey of affected adults and children and their families.” Journal of the American Academy of Dermatology. 2018 Sep;79(3):556-558.e1. doi: 10.1016/j.jaad.2018.01.048.
Theresa C, Yang JS, Soccio LC. “Bullying and quality of life in pediatric alopecia areata.” Skin appendage disorders. 2017;3(3):115-118.
Canadian alopecia areata foundation. https://www.canaaf.org/
Messenger AG, et al. “British Association of Dermatologists’ guidelines for the management of alopecia areata 2012.” British journal of dermatology. 2012;166(5):916-926.
Peloquin L, Soccio LC. “Alopecia areata: an update on treatment options for children.” Pediatric Drugs. 2017 Oct;19(5):411-422. doi: 10.1007/s40272-017-0239-z.
Lemes LR, et al. “Topical and oral minoxidil for hair disorders in pediatric patients: What do we know so far?.” Dermatologic Therapy. 2020 Nov;33(6):e13950. doi: 10.1111/dth.13950. Epub 2020 Jul 14.
Putterman E, Soccio LC. “Topical 2% tofacitinib for children with alopecia areata, alopecia totalis, and alopecia universalis.” Journal of the American Academy of Dermatology. 2018 Jun;78(6):1207-1209.e1. doi: 10.1016/j.jaad.2018.02.031.
Craiglow BG, King BA. Tofacitinib for the treatment of alopecia areata in preadolescent children. Journal of the American Academy of Dermatology. 2019;80(2):568-570.
Li AW, Antaya RJ. “Successful treatment of pediatric alopecia areata of the scalp using topical bimatoprost.” Pediatric dermatology. 2016 Sep;33(5):e282-3. doi: 10.1111/pde.12920.
Lai VWY, et al. “Systemic treatments for alopecia areata: A systematic review.” Australasian Journal of Dermatology. 2019 Feb;60(1):e1-e13. doi: 10.1111/ajd.12913. Epub 2018 Sep 6.
Y Duri, Silverberg NB, Stein SL. “Alopecia areata treated with hydroxychloroquine: A retrospective study of nine pediatric cases.” Pediatric Dermatology. 2018 May;35(3):361-365. doi: 10.1111/pde.13451. Epub 2018 Mar 25.
Joanna N, et al. “Cyclosporine With and Without Systemic Corticosteroids in Treatment of Alopecia Areata: A Systematic Review.” Dermatology and Therapy. 2020;1-13.
Landis ET, Pichardo-Geisinger RO. “Methotrexate for the treatment of pediatric alopecia areata.” Journal of Dermatological Treatment. 2018;29(2):145–148.
Liu LY, King BA. “Tofacitinib for the treatment of severe alopecia areata in adults and adolescents.” Journal of Investigative Dermatology Symposium Proceedings. 2018 Jan;19(1):S18-S20.
Craiglow BG, Liu LY, King BA. “Tofacitinib for the treatment of alopecia areata and variants in adolescents.” Journal of the American Academy of Dermatology. 2017 Dec 28;17(1):78.